The Role of Myelin Sheath in Multiple Sclerosis
The sinusoidal of the life....Viewed: 3834
Posted by: Al Clinics
[email protected]
3347121170
Date: Oct 15 2018 12:28 PM
Multiple Sclerosis
The history of Multiple Sclerosis shows an elusive mystery that has baffled and caused controversy between doctors and scientists alike. The tumultuous history starts with an early case in the 1400’s as described by Medser in 1979. A description of the case of St. Lidwina of Schiedam begins “a woman lost the sight of both eyes and on the next day she lost her speech…on the third day a candlewick was put around her head and she then recovered the sight of one eye and was able to open both…and on (Sunday) she recovered her speech and on the feast of St. Michael…the sight of the eye that has previously been blind.”
Dr. Jean-Martin Charcot (1825-1893) gave the first clinical description of MS in 1873 which he described as “foolish laughter without cause.” About 50 years later in 1926, Cottrell and Wilson published a paper which described four feeling states of well-being observed in MS patients: euphoria sclerotica in which the patient is constantly cheerful, eutonia sclerotica in which the patient is oblivious or apathetic towards his/her disability, spes sclerotica in which the patient has an abnormal positive mindset about the future and his/her ultimate recovery, and emotionally labile. Previously, MS was referred to as Angular Sclerosis, Lobular and Diffuse Sclerosis, and Disseminal Sclerosis which was the most preferred name. The term Multiple Sclerosis, termed in Germany, was not used until the 1950’s.
Clinical Features and Treatments
The essential feature of MS is that the symptomatic episodes are “separated in time and space,” that is episodes that are months or years apart and effect different anatomical locations. In addition, the duration of the attack should be longer than 24 hours. The classical MS symptoms are as follows: paresthesias (sensory loss), motor symptoms such as cramps, spasticity, paresis, and paralysis, spinal cord symptoms such as bladder, bowel, and sexual dysfunction, optic neuritis, cerebellar symptoms including ataxia and tremor, trigeminal neuralgia, facial myokymia, heat intolerance, pain, neurocognitive difficulties like euphoria (Charcot’s “foolish laughter without cause”) and labile moods, depression, bipolar symptoms, and dementia.
Treatments of MS include:
- Plasma exchange (plasmaphoresis)
- Symptomatic management of muscle spasms, bladder control, sexual disfinction, and incontinence
- Immunosuppressants which slow MS progression such as Cytoxan and Imuran
- IV steroids
- Immuno-modulators such as glatiramer (copaxone)
- Treatment of underlying psychiatric issues such as bipolar disorder, depression, dementia, and anxiety
Etiology
Not only a disease of the immune system, MS and its cause remains unclear. The following etiologies have emerged in the last decade or so:
- Demyelination
- Role of immune system
- Genetic Susceptibility
- Environmental Factors
Demyelination
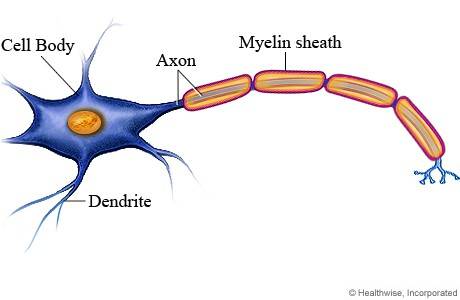
Most mammalian nerve fibers are insulated by myelin to prevent signal loss or crossing. The myelin sheath maintains the electrical signal within the neurons. It also increases the conduction speed in the axon.
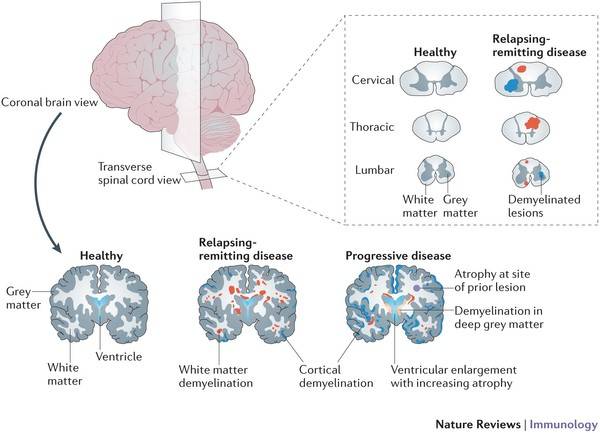
Myelin is produced by oligodendrocytes in the central nervous system (CNS) and Schwann cells in the peripheral nervous system. There are small breaks in the myelin sheath called nodes of Ranvier. In MS, the body mounts an immune response against its own myelin, leading to the destruction of this insulating substance, called demyelination. The demyelination in MS involves the brain and the spinal cord. Because of that, patients with MS experience a diversified variety of symptoms including motor, sensory, vision, cognitive, neuropsychiatric, balance, and incontinence.
MS pathology is characterized by the demyelinated areas in the white and grey matter of the brain and spinal cord. The demyelinated areas are called plaques that indicate the loss of myelin sheath and oligodendrocytes.
Role of the Immune System
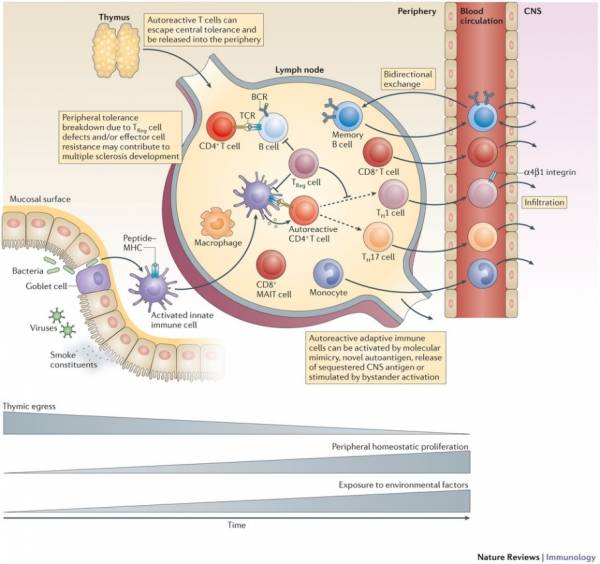
MS is an autoimmune disease, specifically considered CD4+ Th1-mediated. Research performed during the last decade, however, has shown that in addition to CD4+ T cells, other immune factors are involved, including B cells and regulatory cells. The thymus, where T cells mature, is a gland located in front of the pericardium. During the process of central tolerance, auotoreactive T cells are deleted in the thymus. This process is flawed, and as a result, these T cells escape into the periphery
The presence of T cells in the CNS lesions is detectable in the early stages of MS. The main target of these autoreactive T cells are thought to be myelin protein-derived antigens, such as myelin basic protein (MBP), proteolipid protein and myelin oligodedrocyte glycoprotein (MBP), and proteolipid protein and myelin oligodendrocyte glycoprotein (MOG) which all have been shown to be recognized by CD4+ T cells. The main CD4+ T cells found in this disease are Th1 and Th17 cells. Therapies for MS are aimed at steering T cell differentiation instead towards the Th2 phenotype. CD8+ T cells are more frequent than CD4+ cells in the white and grey matter demyelinating regions. CD8+ cells are also positively correlated with axonal damage, and therapies targeting these cells are a possibility for future study. The number of autoreactive B cells, as opposed to T cells, change throughout the development of MS. Studies show, however, that modulating B cell subtypes in the periphery can have a therapeutic effect.
Genetic Susceptibility
Several epidemiological studies show that the increase in frequency of MS seen in the relatives of those afflicted are predominantly caused by genetic factors. Variations within the Major Histocompatibility Complex (MHC) show the highest effect on the risk of having MS. 20 other loci associated with risk have been identified, and these results are showing that multiple variants are exerting different effects which are imperative in the susceptibility of MS.
Environmental Factors
Autoreactive T cells are often triggered by viral and microbial particles. CNS-tropic infectious agents may promote the release of sequestered CNS antigen into the periphery (Theiler’s murine encephalomyelitis virus infection model). There is evidence that high levels of Ebstein Barr Virus specific antibodies increase the risk of MS, so does a history of infectious mononucleosis. Chronic viral infection can lead to an increase in the numbers of virus-specific memory T cells, and this increase may be extenuated in MS. Changes in the gut microbiota can alter the incidence and severity of CNS inflammation. It has been hypothesized that gastrointestinal microbiota might play an important role in the pathogenesis of MS. The studies have demonstrated that MS patients have distinct fecal microbiome compared to healthy controls, with certain microbes either increased or decreased in MS patients compared to controls.
Theiler’s Murine Encephalomyelitis virus (A model for MS). Theiler’s virus, a picorna virus, induces in susceptible strains of mice early acute disease resembling encephalomyelitis followed by late chronic demyelinating disease is one of the best animal model for MS. Two weeks post infection, late chronic demyelinating disease becomes clinically apparent and characterized by demyelinating lesions, progressive spinal cord atrophy and axonal loss. The common features form the basis of close similarities of Theiler’s virus induces demyelinating disease in mice and MS in humans. The virus was first reported by Theiler in 1937 the virus was discovered during research on polio-virus like paralysis symptoms in mice. The same year Theiler completed work on vaccine development for yellow fever and in 1951 received the Noble prize for it.
Summary
Multiple Sclerosis is an immune mediated disease, the etiology of which involves both genetic and environmental factors. Onset of the illness is typically between the age of 25 and 35 and it is far more frequent in women than in men and it is the most common autoimmune disorder affecting the central nervous system with about 2.3 million people affected globally Diagnosis is typically based on signs and symptoms in combination with MRI of the brain, visual and sensory evoked potential and CSF analysis. Just 20 years ago there was no drug treatment options for MS but today there is a wide variety of FDA approved drugs Disease modifying agents like beta – interferon, Copaxone, Glatopa, Gilenya and many others delay the disease progression and reduce or prevent attacks.
Citations
Dendrou, C. A., Fugger, L., & Friese, M. A. (2015). Immunopathology of multiple sclerosis. Nat Rev Immunol Nature Reviews Immunology, 15(9), 545-558. doi:10.1038/nri3871
Fogel, B. S., Schiffer, R. B., & Rao, S. M. (1996). Neuropsychiatry. Baltimore: Williams & Wilkins.
McApline, D., & Compston, A. (1998). McAlpine’s Multiple Sclerosis. London. Churchill Livingstone.
Neuron. Retrieved October 07, 2016. https://myhealth.alberta.ca/Health/tests-treatments/pages/conditions.aspx?hwid=tp12596
Rao, Stephen M. (1990). Neurobehavioral Aspects of Multiple Sclerosis. New York. Oxford University Press.
Sawcer, S., Hellenthal, G., Pirinen, M., Spencer, C. C. A., Compston, A. (2011). Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature, 476(7359), 214–219. http://doi.org/10.1038/nature10251
Sospedra, M., & Martin, R. (2016). Immunology of Multiple Sclerosis. Seminars in Neurology Semin Neurol, 36(02), 115-127. doi:10.1055/s-0036-1579739
Copyright. A part of the article can be used under Fair use policy. Permission needed to reproduce the article. To seek the permission; please send an email to [email protected]

<- back
Rules
1. You may disagree with, but not demean other commenters
2. Do NOT use all caps
3. No unsubstantiated facts
4. NO profanity
5. Stay on topic!
6. All comments are moderated, and approved by the web master
In order to post comments on articles, you must first have an account. Please create an account by clicking the link below, you will then be able to come back to this article to post a comment.


.jpg)









.jpeg)






.jpeg)






 (1).gif)




1.jpg)




1.jpg)








 (2)1.jpg)
.jpg)






1.jpeg)
.jpg)




.jpg)







 (2).jpg)





.JPG)

.jpg)



1.jpg)